

Waystar is a healthcare revenue cycle management platform designed to help organizations manage billing, claims, and payment workflows across high transaction volumes. It primarily serves mid-sized to large provider organizations that need standardized claims processing, denial management, and financial reporting.
This review examines how Waystar performs in real-world settings, particularly for teams evaluating usability, pricing transparency, and workflow fit. It explores where the platform may fall short for intake-focused or behavioral health organizations that depend on real-time eligibility decisions during admissions—and explains why VerifyTreatment may be a stronger choice for teams needing immediate eligibility clarity at first contact.
VerifyTreatment works directly with behavioral health treatment providers to solve eligibility, coverage, and financial clearance challenges that directly impact admissions and revenue. Our platform supports real-time eligibility checks across payers, payer risk alerts, batch verification, insurance discovery, and admissions-ready exports. With hands-on experience supporting inpatient psychiatric and residential treatment workflows, we understand where general medical RCM platforms often miss the mark for behavioral health teams.
Waystar is a cloud-based revenue cycle management platform that helps healthcare providers manage administrative and payment workflows through claim reimbursement. Formed in 2017 through the merger of Navicure and ZirMed—two established healthcare payment companies founded in the late 1990s—Waystar positions itself as an end-to-end solution covering financial clearance, charge capture, claim submission, payer payments, denial management, and analytics.

The company serves thousands of clients representing over 1 million distinct providers and processes over 6 billion healthcare payment transactions annually. Waystar’s value proposition centers on reducing administrative burden and improving financial performance through a centralized platform powered by AI and automation, rather than disconnected point solutions.
Waystar works well for healthcare organizations processing moderate to high claim volumes that need a centralized platform for billing, payments, and revenue cycle reporting. It’s commonly used by ambulatory surgery centers, clinical laboratories, federally qualified health centers (FQHCs), and home health or hospice providers. Mid-sized to large organizations with dedicated billing teams typically benefit most from its breadth and consolidation capabilities.
Waystar may be less suitable for smaller practices or organizations with specialized, admissions-driven workflows. User feedback indicates that implementation, integration, and optimization can require considerable time and internal resources. Practices relying heavily on real-time eligibility verification during intake or needing fast deployment with minimal configuration may find the platform more complex than necessary.
Waystar does not publicly disclose pricing on its website, requiring organizations to contact sales for a demo and custom quote.
While Waystar offers a broad, end-to-end revenue cycle management platform, several limitations emerge when evaluating real-world usage, pricing transparency, and user feedback. These considerations may affect how well the platform fits certain organizations, particularly smaller teams or those with specialized workflows.
Some organizations report longer-than-expected implementation timelines, particularly when integrating Waystar with existing EMRs or migrating clearinghouse workflows. This can be challenging for teams without dedicated technical or billing resources.
For behavioral health providers, this pricing opacity can be especially challenging. Admissions volume often fluctuates, payer mix varies by state, and verification needs can change rapidly. Without upfront pricing clarity, smaller or growing facilities may struggle to evaluate the total cost of ownership or compare Waystar accurately against verification-first alternatives.
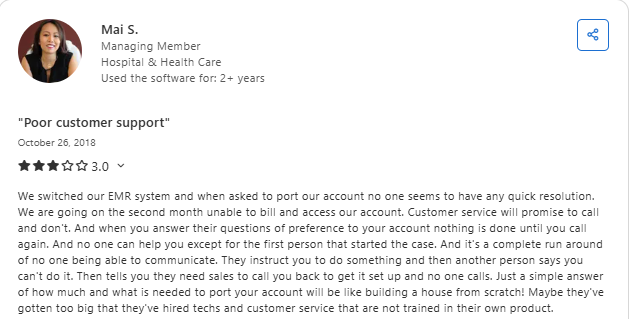
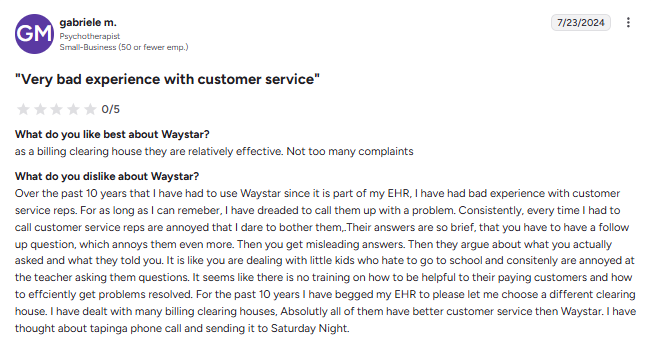
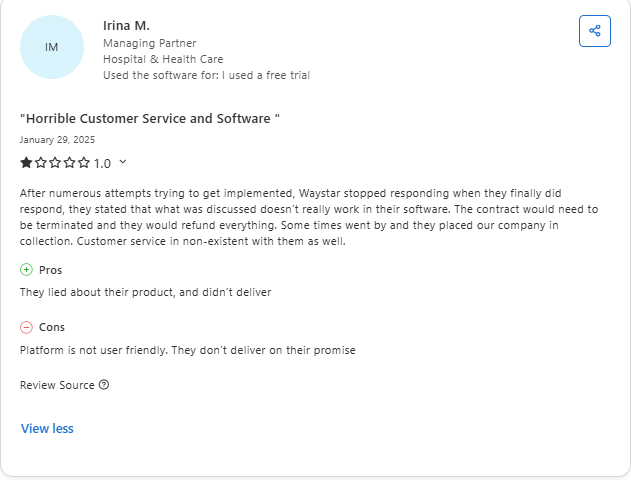
Some reviewers report inconsistent customer support experiences, particularly during implementation, account changes, or urgent billing disruptions.
While generally considered easy to use, some users note workflow inefficiencies, visibility limitations, and interface behaviors that can slow day-to-day operations.
Behavioral health programs frequently encounter payer-specific carve-outs, managed care rules, and state-level Medicaid variations. When eligibility results lack this depth, teams must revert to manual portal checks or payer calls, reintroducing delays, increasing staff burden, and undermining real-time intake decisions.
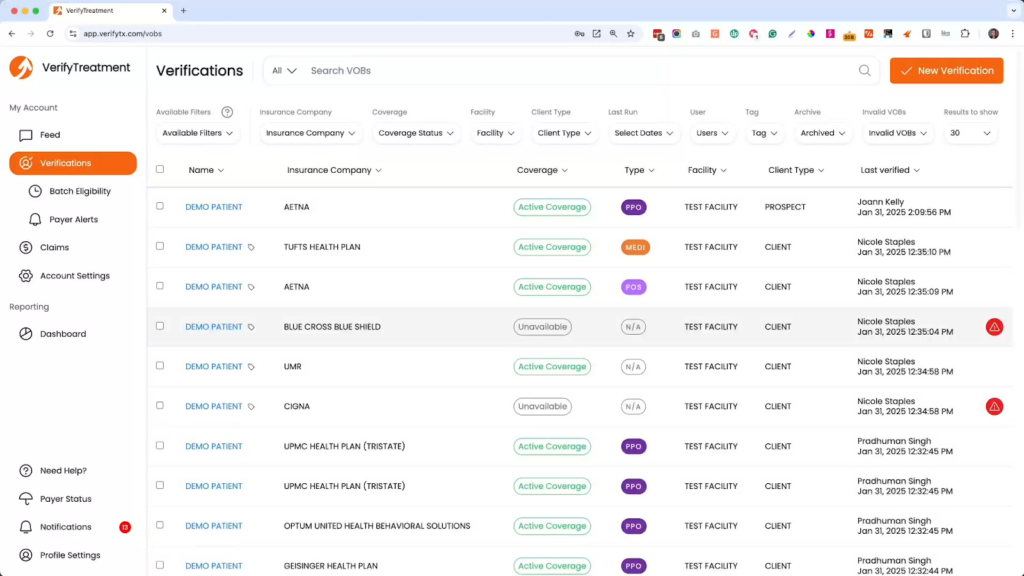
VerifyTreatment is a verification-first healthcare platform designed to help practices manage eligibility, coverage, and payer risk more efficiently than general revenue cycle solutions. Its tools are built to reduce manual verification work, provide reliable visibility into patient insurance status, and streamline workflows across admissions, billing, and utilization review teams.
Real-time eligibility checks, insurance discovery, payer alerts, and batch re-verification help prevent denials before they occur and provide teams with clear, actionable financial visibility at the point of intake—when admission decisions are made.
| Criteria | Waystar | VerifyTreatment |
| Ease of use and setup time | More complex onboarding; learning curve for non-billing staff | Fast setup; intuitive for admissions teams |
| Support responsiveness and customer experience | Inconsistent support reported by some users | Hands-on onboarding and responsive support |
| Transparency and operational clarity | Data-rich, but often requires interpretation | Clear, admissions-ready benefit summaries |
| Handling of edge cases and exceptions | Manual follow-up often required | Behavioral health–specific flags surfaced upfront |
| Flexibility for smaller or specialized practices | Better suited to larger, billing-heavy organizations | Flexible for small, mid-size, and specialty providers |
| Workflow alignment with admissions and frontend teams | Billing- and back-end–oriented | Built for front-end and intake workflows |
| Integration consistency across systems | Depends heavily on EMR and clearinghouse setup | Works alongside EMRs without dependency |
Waystar excels at back-end revenue cycle operations—claims processing, payment management, and denial recovery after admission. This approach works well for organizations with established billing departments but treats eligibility verification as an early checkpoint rather than a critical intake decision point.
VerifyTreatment prioritizes the intake conversation. It delivers behavioral health-specific coverage details, authorization requirements, and payer risk signals in real time, enabling admissions teams to make confident decisions immediately—even during high-volume periods or after hours.
For behavioral health providers, this distinction matters. Delays or coverage misinterpretations at intake lead to lost admissions, downstream denials, and preventable write-offs. When evaluating platforms, consider not just post-admission workflows, but how quickly and accurately you can make coverage decisions before accepting a patient.
VerifyTreatment allows admissions teams to verify coverage in real time during the first call, reducing delays and lost admits. Teams can see deductibles, copays, carve-outs, and authorization needs immediately, including payer nuances like Medicaid, Medicare Advantage, and BCBS alpha prefix variations.
Built for admissions teams, not billing specialists, VerifyTreatment requires minimal setup and training. Most facilities can begin verifying benefits within days using only their NPI, without complex configuration or technical overhead.
Benefit information is presented in a clear, admissions-ready format that highlights patient responsibility and coverage limits early. This reduces internal handoffs, miscommunication, and financial surprises after admission.
VerifyTreatment flags common eligibility risks before admission, such as inactive policies, out-of-network coverage, behavioral health carve-outs, and missing authorizations—helping reduce denials and protect revenue.
Eligibility goes beyond active/inactive status, surfacing behavioral health carve-outs, authorization requirements, plan type distinctions, and payer-specific nuances like Medicaid, Medicare Advantage, and BCBS alpha prefixes, so admissions teams get clear answers at intake.
Waystar is a solid choice for healthcare organizations that prioritize standardized billing operations, centralized claim management, and back-end revenue cycle optimization. Large multi-specialty systems or providers with established billing departments may find its clearinghouse capabilities and reporting tools reliable for managing high claim volumes across payers.
For behavioral health providers where admission speed, eligibility clarity, and payer nuance directly impact revenue, VerifyTreatment is often the stronger fit. Teams that verify benefits during the first call, operate after hours, or regularly encounter behavioral health carve-outs and authorization issues benefit from a platform built specifically for front-end decision-making rather than retrofitted billing workflows.
The choice ultimately comes down to where revenue protection happens in your organization. If your biggest risk is inaccurate intake decisions that lead to denials, lost admissions, and write-offs, a verification-first platform designed for behavioral health will deliver better outcomes than a general RCM solution built for post-admission workflows.
If protecting revenue at intake is a priority, try VerifyTreatment as a purpose-built alternative.



Samantha is a dynamic marketing professional dedicated to making a difference in the behavioral health industry through her work at VerifyTreatment. With a strong background in digital marketing and brand advocacy, she helps elevate the platform’s presence by fostering authentic connections with treatment centers and healthcare providers. Her expertise in content creation and community engagement ensures that VerifyTreatment’s value is communicated effectively, helping centers streamline operations and improve patient care. Samantha’s focus on building trust and driving awareness positions VerifyTreatment as a key resource in the healthcare landscape.

Nicole is a versatile healthcare professional with a Bachelor’s degree in Health Administration and a solid background in managing healthcare systems and operations. Her experience spans healthcare management, compliance, and regulations, making her adept at navigating complex healthcare environments. In addition to her administrative expertise, Nicole holds certifications in Functional Nutrition and Personal Training, giving her a well-rounded perspective on health and wellness. She is committed to using her skills to improve healthcare settings and ensure effective, patient-centered care.

Tara is a dedicated leader who leverages her Master's degree in Information Technology (Florida Tech) and deep company knowledge (since 2018) to drive our community awareness. She is the central figure for managing social engagement and ensuring the community is immediately and effectively informed of all new product launches and company updates.

JoAnn has a strong background in the mental health and substance abuse industry, with expertise in billing, coding, facility credentialing, and contracting. She is passionate about team education and public speaking, always striving to make a positive impact. With a solid foundation in accounting, JoAnn also holds an Associate of Arts in Biblical Studies from Liberty University, blending her professional skills with her personal values.

For 11+ years, Melanie has been dedicated to helping clients access quality mental health care, with a special focus on grief, loss, and substance abuse. With expertise in healthcare, community outreach, patient advocacy, and leadership development, Melanie is passionate about making a positive impact in the lives of others.

Jordan is a dedicated advocate for behavioral health and is passionate about improving sales strategies and business processes. With a focus on helping businesses, particularly in healthcare, Jordan believes that streamlining operations is a way to positively impact more people indirectly. A strong leader, both personally and professionally, Jordan is committed to making a difference in the world by doing good business and serving a higher purpose.