

Availity serves as a central hub for administrative and clinical data exchange between healthcare providers and insurance payers, helping streamline workflows, reduce manual processes, and minimize errors across multiple payer networks.
This review examines Availity’s core features, pricing structure, and real-world user feedback to help healthcare providers determine if the platform meets their verification and revenue cycle needs. We also explore alternative solutions, including VerifyTreatment, for providers who require more specialized insurance verification capabilities.
VerifyTreatment was built by healthcare providers who experienced firsthand the operational challenges of insurance verification—denied claims, verification delays, and revenue loss from coverage gaps. Our team helps facilities ensure proper insurance coverage before admission, reducing unrecoverable losses and streamlining verification workflows.

“Great Product, Ease of Use, Added Efficiency for Our Team. Automating and bringing in health insurance verifications to our instance was a game changer. We have instant verifications for all of our prospects, as well as automated verifications for our clients on a weekly basis.”
We understand the pain points because we’ve lived them. That’s why this review examines Availity honestly—acknowledging where it excels and where providers might need more specialized solutions. Our goal is to help you make an informed decision based on your facility’s actual verification needs.
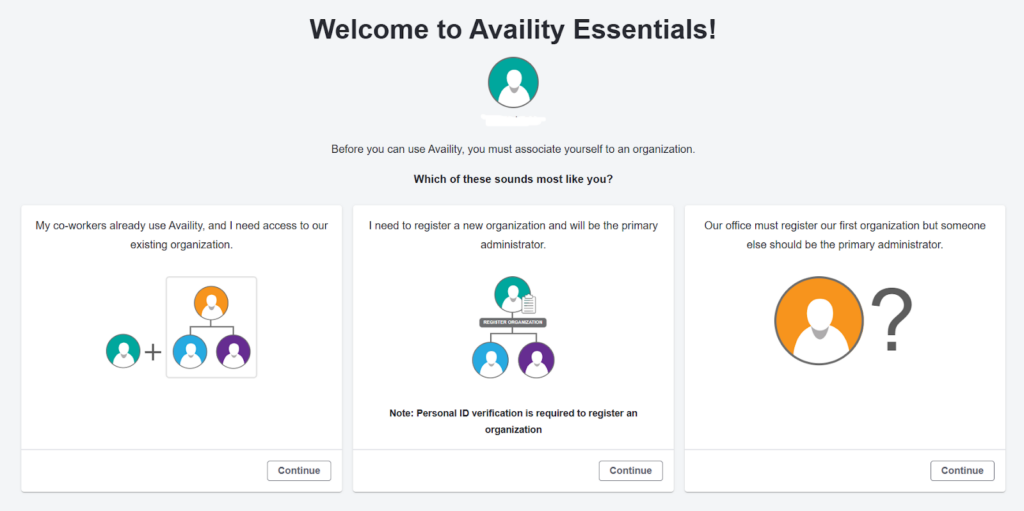
Availity is a health information network that facilitates data exchange between healthcare providers, health plans, and technology partners. The platform centralizes administrative functions like eligibility verification, claims submission, and prior authorizations across multiple insurance payers.
As the nation’s largest real-time health information network, Availity processes 13 billion clinical, administrative, and financial transactions annually. The platform addresses a fundamental challenge in healthcare: the need for providers to communicate with dozens of different insurance companies through a single, standardized interface.
Availity is designed for:
Availity is not ideal for:
For Providers:
For Payers:
For HITs:
Availity does not publish transparent pricing on its website. To access detailed cost information, providers must create an account or contact the sales team directly. This lack of pricing transparency makes it difficult to budget for the platform or compare costs against alternatives.
The most recently published pricing tiers (last updated in 2023) include:
Given that this pricing is now three years old and Availity has not published updated rates, providers should contact Availity directly for current pricing. The free tier makes the platform accessible to small practices, but the lack of transparency around paid features and their costs remains a barrier to informed decision-making.
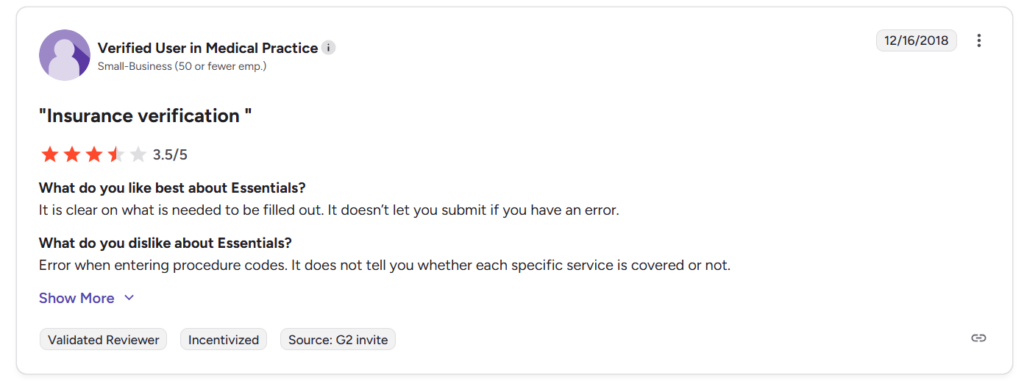
Users report that claims and payment information cannot always be located within the system, requiring them to contact payers directly or use alternative methods. Some providers note that access to out-of-state Blue Cross Blue Shield claims, previously available, has been restricted. Additionally, insurance card details and policy information don’t consistently work across all insurance companies, leading to incomplete verification data.
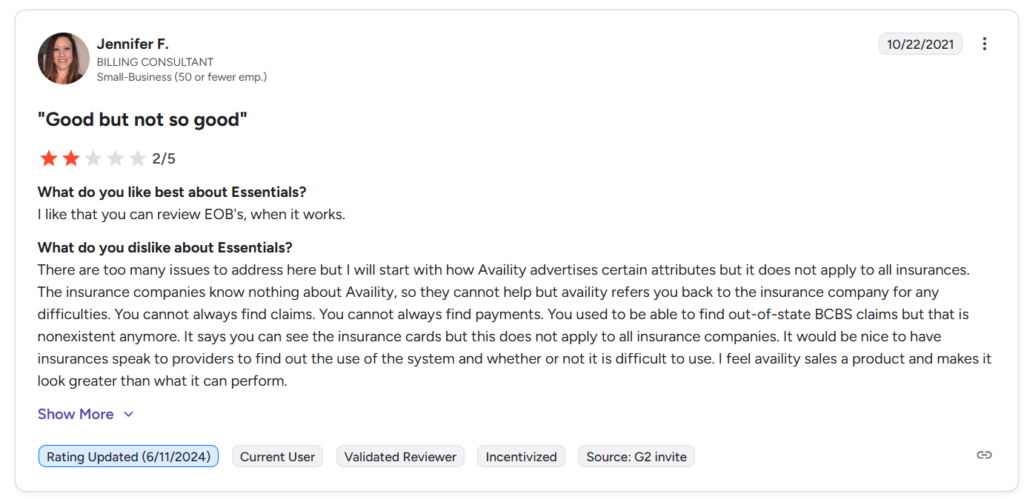
Navigation remains a consistent complaint among users. Providers describe the interface as difficult to navigate, with multiple reviewers explicitly stating the platform is “not user-friendly.” Basic tasks that should be straightforward often require workarounds or multiple steps, suggesting the platform may not have been designed with actual end-user workflows in mind.
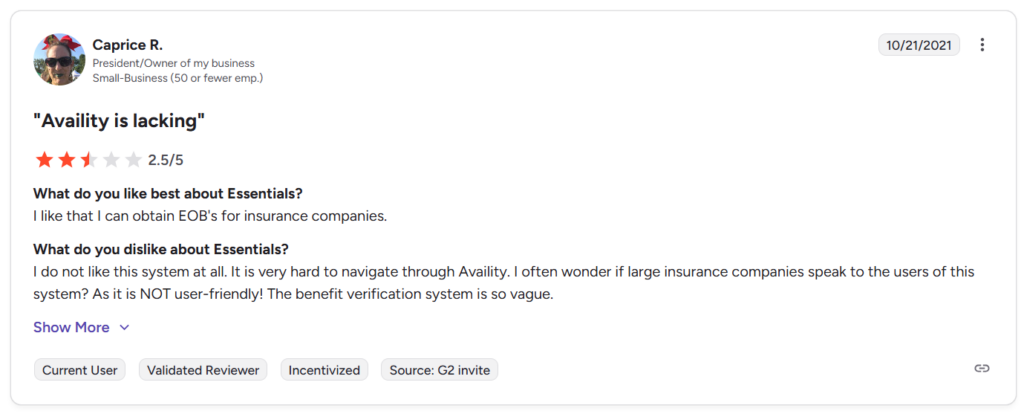
Availity advertises comprehensive benefit verification, but users report that the system provides vague coverage information. The platform often doesn’t clearly indicate whether specific services or procedure codes are covered, forcing providers to make additional calls to payers for confirmation. This gap between advertised capabilities and actual functionality creates frustration, particularly for providers who need detailed verification before admitting patients.
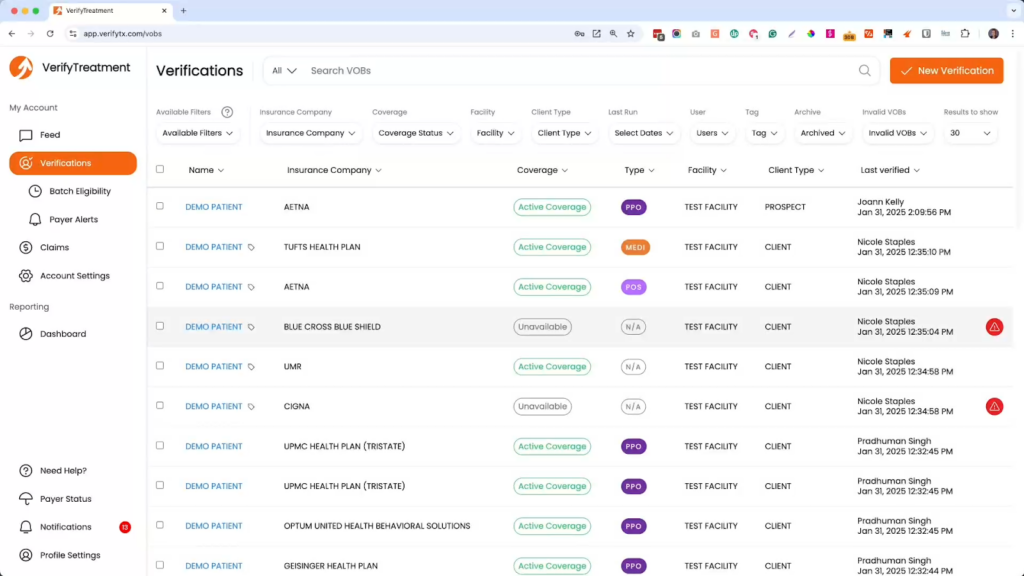
For providers who require more detailed, service-level insurance verification—particularly in behavioral health and specialty care—VerifyTreatment offers a platform built specifically for pre-admission verification workflows.
VerifyTreatment focuses on behavioral health facilities, skilled nursing centers, durable medical equipment (DME) providers, billing companies, and revenue cycle management firms. The platform is designed to provide the depth of coverage information and verification clarity that general-purpose networks often lack.
Here’s a quick summary of how each platform compares on usability, reliability, and feature clarity:
| Category | Availity | VerifyTreatment |
| Ease of Use | Users frequently report navigation difficulties and a steep learning curve | Streamlined interface designed specifically for verification workflows |
| Insurance Verification Clarity | Provides basic eligibility but often lacks service-level coverage details | Delivers detailed, behavioral health-specific benefit information before admission |
| Error Prevention | Errors can occur with procedure codes and unclear coverage feedback | Payer alerts and verification depth help prevent common submission errors |
| Coverage Consistency | Varies across insurance companies and regions; some payers provide limited data | Focused verification process designed to catch coverage gaps before admission |
| Feature Transparency | Advertised features don’t always apply to all connected insurance providers | Clear indication of which payers and verification types are supported |
| Data Reliability | Claims, payments, and insurance details are not always accessible within the platform | Focused on ensuring complete verification data is captured upfront |
| Batch Processing | Not available for verification workflows | Batch verification for multiple patients simultaneously |
VerifyTreatment was developed by healthcare professionals who experienced the daily challenges of admissions, billing, and reimbursement in behavioral health. The platform addresses real operational problems: incomplete verification leading to denials, time-consuming manual processes, and lack of service-level coverage clarity. The platform includes HIPAA-compliant team messaging, allowing verification teams to communicate securely without leaving the system.
Unlike platforms where essential features are locked behind premium tiers, VerifyTreatment’s pricing plans provide meaningful functionality at each level. Providers receive verification capabilities that align with their tier’s cost, rather than paying for access to features that should be standard for effective insurance verification.
The batch verification feature allows teams to verify multiple patients simultaneously with supported payers, reducing the time spent on repetitive, individual verification tasks. This efficiency gain allows staff to focus more time on patient care and complex cases that require individual attention.
By providing clearer visibility into coverage details and service-level benefits, VerifyTreatment helps providers make informed admission decisions. When verification is more complete upfront, facilities avoid the operational and financial disruption of post-admission denials and can ensure patients have confirmed coverage before beginning treatment.
Availity remains a widely used platform for provider-payer communication, offering a centralized hub for eligibility checks, claims submission, authorizations, and digital correspondence across multiple health plans. For providers who need basic eligibility verification and claims management across a broad payer network, Availity serves its purpose effectively.
However, as verification requirements grow more complex—particularly in behavioral health and specialized care settings—Availity’s limitations become more apparent. The platform’s lack of service-level coverage details, inconsistent data availability across payers, and navigation challenges can create operational friction for facilities that need detailed verification before admission.
For organizations operating within Availity’s established payer network and requiring only basic eligibility checks, the platform remains a viable option. But for providers that need detailed, service-level insurance verification to prevent denials and manage high patient volumes, a more specialized solution may be necessary.
VerifyTreatment addresses these gaps by focusing exclusively on insurance verification. Its payer alerts, batch verification capabilities, workflow integrations, and transparent pricing help teams make informed admission decisions, protect revenue, and reduce operational friction. For organizations where verification accuracy directly impacts financial performance, VerifyTreatment offers a solution built specifically for that challenge.




Samantha is a dynamic marketing professional dedicated to making a difference in the behavioral health industry through her work at VerifyTreatment. With a strong background in digital marketing and brand advocacy, she helps elevate the platform’s presence by fostering authentic connections with treatment centers and healthcare providers. Her expertise in content creation and community engagement ensures that VerifyTreatment’s value is communicated effectively, helping centers streamline operations and improve patient care. Samantha’s focus on building trust and driving awareness positions VerifyTreatment as a key resource in the healthcare landscape.

Nicole is a versatile healthcare professional with a Bachelor’s degree in Health Administration and a solid background in managing healthcare systems and operations. Her experience spans healthcare management, compliance, and regulations, making her adept at navigating complex healthcare environments. In addition to her administrative expertise, Nicole holds certifications in Functional Nutrition and Personal Training, giving her a well-rounded perspective on health and wellness. She is committed to using her skills to improve healthcare settings and ensure effective, patient-centered care.

Tara is a dedicated leader who leverages her Master's degree in Information Technology (Florida Tech) and deep company knowledge (since 2018) to drive our community awareness. She is the central figure for managing social engagement and ensuring the community is immediately and effectively informed of all new product launches and company updates.

JoAnn has a strong background in the mental health and substance abuse industry, with expertise in billing, coding, facility credentialing, and contracting. She is passionate about team education and public speaking, always striving to make a positive impact. With a solid foundation in accounting, JoAnn also holds an Associate of Arts in Biblical Studies from Liberty University, blending her professional skills with her personal values.

For 11+ years, Melanie has been dedicated to helping clients access quality mental health care, with a special focus on grief, loss, and substance abuse. With expertise in healthcare, community outreach, patient advocacy, and leadership development, Melanie is passionate about making a positive impact in the lives of others.

Jordan is a dedicated advocate for behavioral health and is passionate about improving sales strategies and business processes. With a focus on helping businesses, particularly in healthcare, Jordan believes that streamlining operations is a way to positively impact more people indirectly. A strong leader, both personally and professionally, Jordan is committed to making a difference in the world by doing good business and serving a higher purpose.