

Waystar and Availity both streamline revenue cycle tasks that would otherwise drain hours, including eligibility checks, claims, denials, and payer follow-ups. But they solve these problems differently. Waystar functions as a full RCM engine powered by automation and AI, while Availity operates as a massive connectivity hub with broad payer access. For behavioral health providers, neither fully addresses carve-outs or rapid admissions the way VerifyTreatment does.
If tools like Waystar and Availity didn’t exist, you’d spend hours every week chasing eligibility, calling payers, correcting preventable denials, and watching cash flow slow to a crawl. Both platforms exist to take that burden off your team but they’re not built the same.
Waystar leans toward automation, AI, and deeper revenue-cycle control, while Availity centers on connectivity — a massive network linking providers and payers. And depending on your size and workflow, one may fit naturally, while the other may feel heavier than you need.
If you’re comparing both to see which actually makes your operations easier, this breakdown gives you the clarity you’re looking for.
We work with admissions and RCM teams every day — the same teams trying to choose between tools like Waystar and Availity. VerifyTreatment was built to solve the specific problems they kept running into: slow verifications, missing behavioral health details, coverage changes, and denials that could have been prevented.
One facility, Foundations Recovery Network, recovered $10,000+ in monthly revenue simply by closing these gaps with VerifyTreatment.
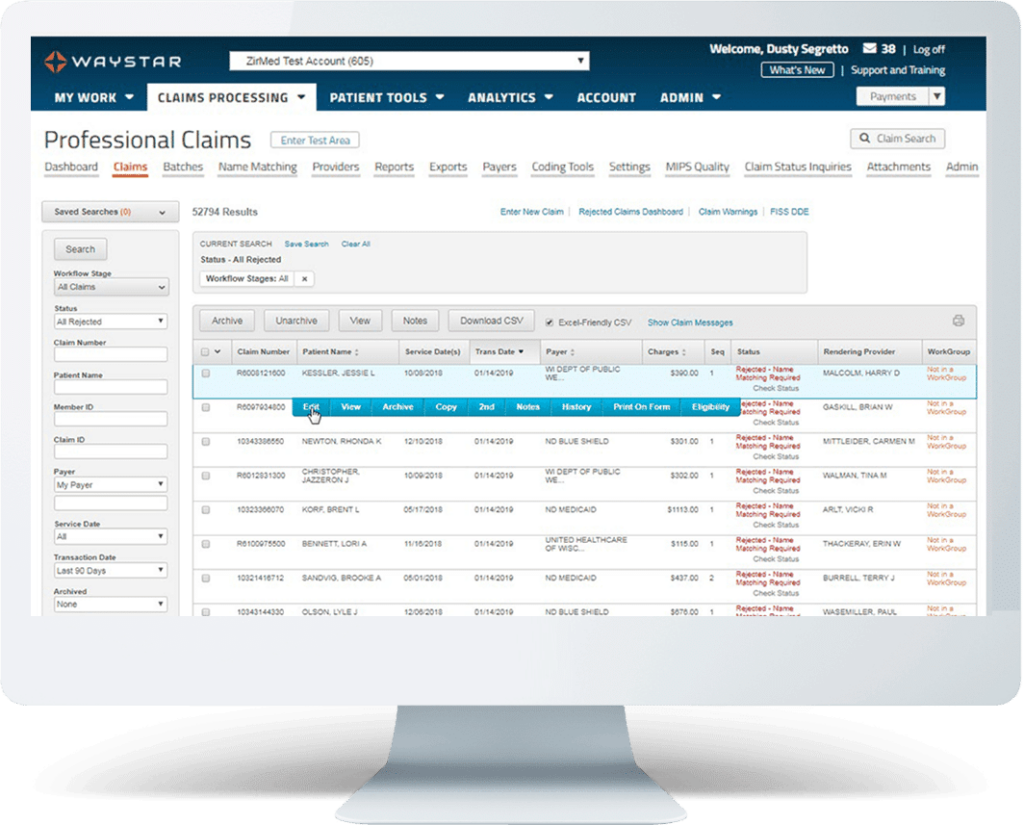
Waystar is the all-in-one control center for revenue cycle teams that want fewer denials, cleaner claims, and a workflow that catches mistakes before payers ever see them. Its Claims Manager scrubs, edits, and predicts denials before submission, reducing backend rework. Its Eligibility + Coverage Detection normalizes payer data so you see accurate benefits in one place, without jumping between portals. And tools like AltitudeAI and Rules Manager automate corrections, surface missing information, and accelerate reimbursement.
Availity, meanwhile, is built for sheer connectivity. Its real-time EDI network lets you check eligibility, claims, and remits from one login, while payer-spaces and APIs plug you into a massive nationwide network. As one reviewer put it, Availity brings “claim status and eligibility from multiple payers… in one space, with one login.”
Even though user reviews rarely talk about “AI” directly, you can clearly see Waystar’s strategy: automate the revenue cycle so your team does less manual cleanup. Its AltitudeAI™ suite is built around three pillars — AltitudeCreate™, which generates cleaner claim content and documentation; AltitudeAssist™, which automates corrections and flags missing data; and AltitudePredict™, which forecasts denials before they happen. Together, these tools reduce the grunt work that normally slows down RCM teams and improve first-pass yield.
Availity, on the other hand, also uses automation and predictive editing but not at the same depth or positioning as Waystar. Instead, Availity’s real value comes from its network: its payer connections, its real-time EDI rails, its payer-spaces integrations, and its APIs that reduce back-and-forth friction. Where Waystar tries to replace manual RCM work, Availity tries to simplify the path between you and the payer.
Waystar users consistently highlight how easy it is to submit, track, and correct claims. Its Claims Manager scrubs errors before submission, surfaces payer-specific edits, and gives you clear visibility into how a claim moved through the system. Several users even call it a “life saver” because it catches problems early and makes it easy to find proof of timely filing.
Availity’s experience is more mixed. While many users appreciate the ability to submit claims across countless payers, others report recurring issues with proof of submission, missing claim history, or claim status showing “no claim on file” even after payment. One biller put it plainly:
“Anything denied for timely filing that went through Availity had to be written off because I couldn’t get proof of the submission.”
If defensible claim submission matters in your workflow, this difference is hard to ignore.
Waystar focuses on depth of eligibility data. Its Eligibility + Coverage Detection engine normalizes messy payer information, fills in missing details, and automatically searches for additional active coverage when something looks off. For many users, this means fewer surprises after admission and fewer denials tied to inaccurate benefit data.

Availity, meanwhile, emphasizes reach. Its dual-sided network gives you eligibility access to an enormous range of payers — often faster than hopping between portals. Many users say Availity is their go-to “quick check” tool because almost every major plan can be verified from a single login.
Support sentiment for both platforms is extremely polarized but in very different ways.
With Waystar, users tend to fall into two camps. Some rave about “great customer service,” fast help, and easy access to support reps. Others describe the experience as “the worst I’ve ever had,” citing unreturned tickets, unhelpful reps, and frustration strong enough that multiple reviewers said they dread calling Waystar. The gap depends heavily on the account, the rep, and how complex your setup is.
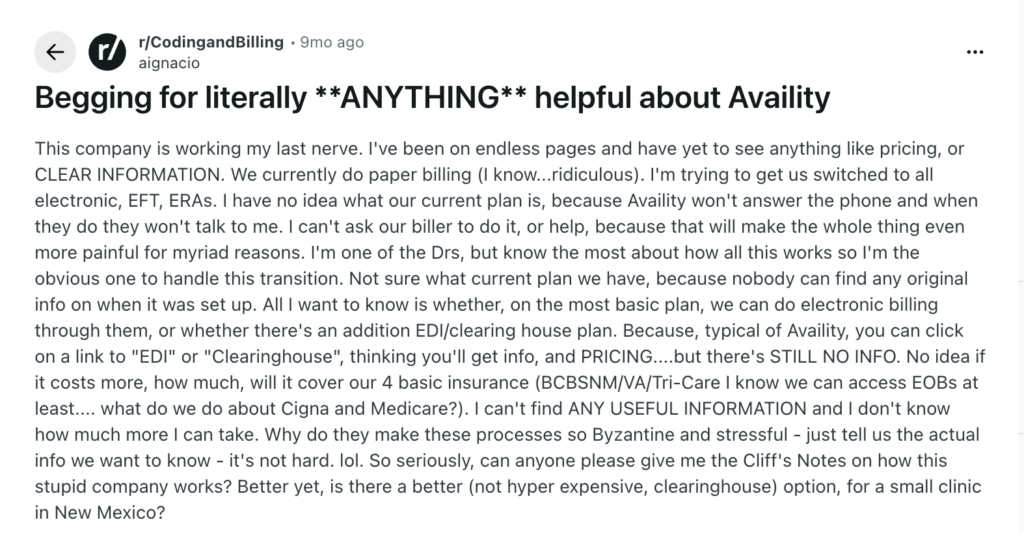
Availity gets the same split — just for different reasons. Many users say support is “excellent,” especially for quick eligibility or claim checks. But a large group complains that Availity simply doesn’t answer, doesn’t clarify pricing or plan tiers, and often redirects users back to the payer when something goes wrong. One reddit user trying to transition from paper billing summed it up: “I can’t get anyone on the phone. I just want clear answers.”
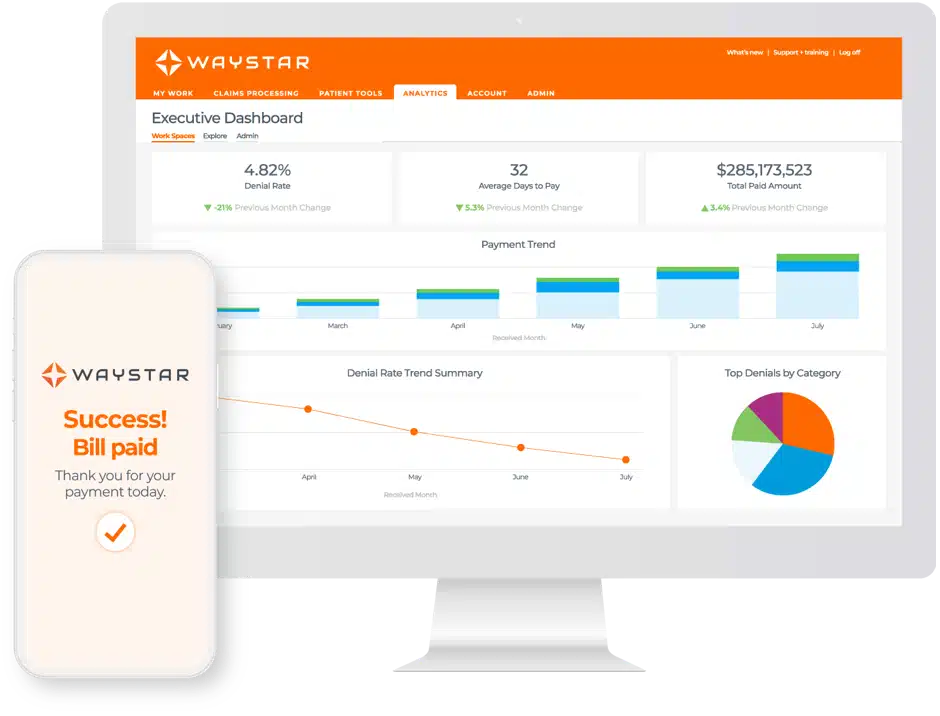
Waystar is a full revenue cycle automation platform designed to help healthcare organizations submit cleaner claims, prevent denials, accelerate payment, and reduce the manual workload that slows down billing teams. It combines clearinghouse functionality with AI-driven workflows, eligibility intelligence, denial prediction, prior authorization automation, and deep analytics — making it one of the most robust RCM engines on the market.
Waystar pricing is not public, but reviewers commonly describe it as more expensive than alternatives, with:
Users consistently advise: “Read the contract closely especially renewal terms and provider counts.”
Availity is a nationwide healthcare connectivity and clearinghouse platform that acts as the central gateway between providers, payers, and HIT systems. Instead of operating like a full RCM engine, Availity focuses on real-time eligibility, claims submission, claim status, remits, and payer-specific workflows—all from a single login. It’s known for its massive payer reach, dual-sided network, and the ability to integrate administrative and clinical data into key transactions.
Availity’s pricing structure is not transparent, and this is one of the most common user complaints. What’s known from reviews and industry patterns:
Here’s a screenshot of a reddit user sharing their frustration:
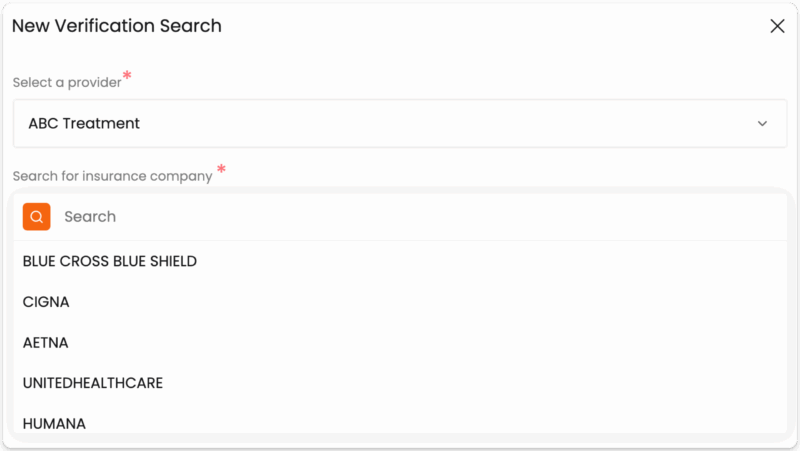
If you look closely at how these platforms work, you will see that Waystar focuses heavily on automation, but it does not reliably expose behavioral health carve-outs or the benefit details admissions teams depend on. Availity, on the other hand, provides strong connectivity to many payers, but when it comes to behavioral health nuance and real coverage clarity, it often leaves teams without the information they need to make the right call at intake.
VerifyTreatment bridges both gaps. It delivers behavioral-health-specific eligibility, real-time coverage monitoring, deep exclusion checks, and instant insight into authorization requirements. It gives admissions and billing teams the clarity they need upfront, instead of discovering problems after the patient is already in care.
VerifyTreatment keeps pricing simple and contract-light:
Most importantly, you don’t get penalized for growth. Adding more verifications or team members doesn’t trigger surprise billing.
| Feature / Capability | Waystar | Availity | VerifyTreatment |
| Primary Purpose | Full RCM automation platform (claims, denials, eligibility, payments) | National connectivity hub + clearinghouse | Behavioral health–specific eligibility intelligence |
| Best For | Mid-to-large practices, health systems, multi-provider RCM teams | Small to large practices needing multi-payer access | Behavioral health, SUD, MH providers focused on admissions + revenue protection |
| Eligibility Detail | Deep, normalized eligibility + coverage detection | Broad payer eligibility access; detail varies by payer | BH-specific benefit detail, carve-outs, auth requirements |
| Carve-Out Detection | Limited; misses BH carve-outs | Limited; dependent on payer integration | Industry-leading carve-out detection (Beacon, Magellan, Optum, etc.) |
| Authorization Tools | Authorization Manager + AI-driven requirements and tracking | Auth submission/status depending on payer | Flags whether auth is required before admission |
| Claims Management | Advanced scrubbing, edits, AI predictions | Standard edits; mixed user experience; proof-of-submission issues | Not a claim-submission tool (pairs with your existing RCM/clearinghouse) |
| Denial Management | Automated appeals, AI letter generation | Basic workflows depending on tier | Prevents denials upfront by catching coverage issues early |
| Batch Verification | Not a core feature | Not offered | Full census checks; continuous policy monitoring |
| Team Collaboration | Inside certain modules; varies | Limited; mostly admin roles | Built-in HIPAA-compliant messaging, tagging, shared VOBs |
| AI Capabilities | Strong: AltitudeAI™, AltitudeAssist™, AltitudePredict™ | Some predictive editing; less emphasized | Focused intelligence for BH workflows |
Waystar and Availity serve the entire healthcare ecosystem. VerifyTreatment, on the other hand, is built for behavioral health, SUD, and mental health admissions. Meaning that it catches the carve-outs, exclusions, and level-of-care nuances the big RCM tools routinely miss.
Most platforms focus on correcting denials after the fact. VerifyTreatment flags missing authorizations, benefit limitations, lapsed coverage, and BH carve-outs before you admit a patient, saving facilities $7,000–$10,000 per avoidable denial.
Slow verification costs admissions. Providers choose VerifyTreatment because it delivers full VOB results in seconds, offers a mobile app for on-the-go checks, and lets teams make fast decisions during the first phone call.
Instead of siloed information, VerifyTreatment gives every department the same real-time data.
Built-in HIPAA-compliant messaging, patient tagging, and shared VOB reports eliminate the “admissions said one thing, billing got another” problem entirely.
Other platforms stop at the first eligibility check. VerifyTreatment’s batch verification + ongoing policy monitoring alerts your team when coverage lapses, when benefits change, or when a payer switches mid-care, protecting revenue every single day of treatment.
Waystar and Availity are strong platforms, but they are built for general medical workflows, large networks, and broad revenue cycle operations. If your organization lives and breathes behavioral health, they will not always catch the details that matter most: carve-outs, exclusions, authorization nuances, and level-of-care differences that determine whether a patient is admitted or whether you get paid.
VerifyTreatment fills that gap. It gives behavioral health providers the speed, accuracy, team alignment, and revenue protection that traditional RCM tools were never designed for. If you want to reduce denials, admit patients faster, and stop losing revenue to preventable mistakes, VerifyTreatment is the purpose-built solution created for exactly that.
Get started with VerifyTreatment Here.



Samantha is a dynamic marketing professional dedicated to making a difference in the behavioral health industry through her work at VerifyTreatment. With a strong background in digital marketing and brand advocacy, she helps elevate the platform’s presence by fostering authentic connections with treatment centers and healthcare providers. Her expertise in content creation and community engagement ensures that VerifyTreatment’s value is communicated effectively, helping centers streamline operations and improve patient care. Samantha’s focus on building trust and driving awareness positions VerifyTreatment as a key resource in the healthcare landscape.

Nicole is a versatile healthcare professional with a Bachelor’s degree in Health Administration and a solid background in managing healthcare systems and operations. Her experience spans healthcare management, compliance, and regulations, making her adept at navigating complex healthcare environments. In addition to her administrative expertise, Nicole holds certifications in Functional Nutrition and Personal Training, giving her a well-rounded perspective on health and wellness. She is committed to using her skills to improve healthcare settings and ensure effective, patient-centered care.

Tara is a dedicated leader who leverages her Master's degree in Information Technology (Florida Tech) and deep company knowledge (since 2018) to drive our community awareness. She is the central figure for managing social engagement and ensuring the community is immediately and effectively informed of all new product launches and company updates.

JoAnn has a strong background in the mental health and substance abuse industry, with expertise in billing, coding, facility credentialing, and contracting. She is passionate about team education and public speaking, always striving to make a positive impact. With a solid foundation in accounting, JoAnn also holds an Associate of Arts in Biblical Studies from Liberty University, blending her professional skills with her personal values.

For 11+ years, Melanie has been dedicated to helping clients access quality mental health care, with a special focus on grief, loss, and substance abuse. With expertise in healthcare, community outreach, patient advocacy, and leadership development, Melanie is passionate about making a positive impact in the lives of others.

Jordan is a dedicated advocate for behavioral health and is passionate about improving sales strategies and business processes. With a focus on helping businesses, particularly in healthcare, Jordan believes that streamlining operations is a way to positively impact more people indirectly. A strong leader, both personally and professionally, Jordan is committed to making a difference in the world by doing good business and serving a higher purpose.